Day 4- Thrombocytopenia
Remember:
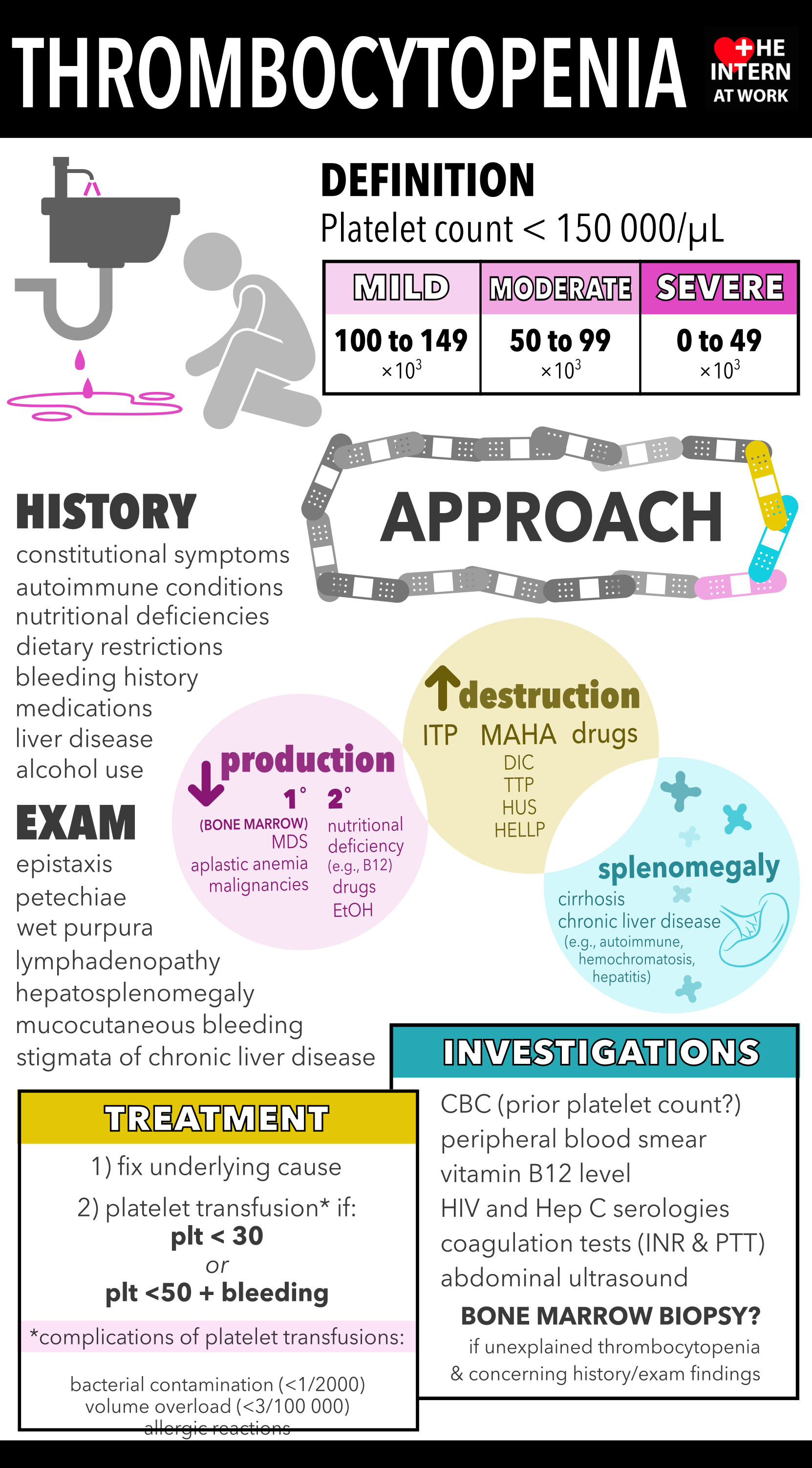
If platelets are low- check previous counts! Is this acute or chronic? Order platelets in a “citrated tube- green top” to rule out pseudothrombocytopenia
platelets <10 puts the patient at risk for spontaneous intracranial bleeding (see other blog post for transfusion thresholds)
safety on anticoagulation should always be questioned when platelets < 30-50
Rule out life-threatening causes: TTP, DIC, leukemias, HIT. Always get a blood film
think about clinical context, severity of thrombocytopenia and time course
TTP and DIC discussed in “hemolytic anemia” blog post
HIT
Clinical-pathological syndrome consisting of thrombocytopenia and positive HIT antibody
More common:
UFH>LMWH
full dose anticoagulation compared to medical prophylactic doses
orthopaedic > cardiac surgery > medical/obstetrical patients
Clinical Manifestations:
causes both venous and arterial thrombosis
may also have skin necrosis at heparin injection sites
Occasionally may present acutely with transfusion reaction immediately after heparin bolus
Time Course:
antibodies to platelets after 5-8 days
typically, platelet begins to drop 5-10 days after heparin exposure (70% of patients)
occasionally may occur immediately after exposure to heparin, in the context of recent exposure to heparin
Diagnosis:
Treatment:
stop heparin
send HIT assay (+/- serotonin release assay)
if strong clinical suspicion, start anticoagulation with non-heparinoid anticoagulant (ie. fondaparinaux)
reassess once assays are back, if serotonin release assay + patient should be advised to avoid heparin for life