Day 2 - Delirium
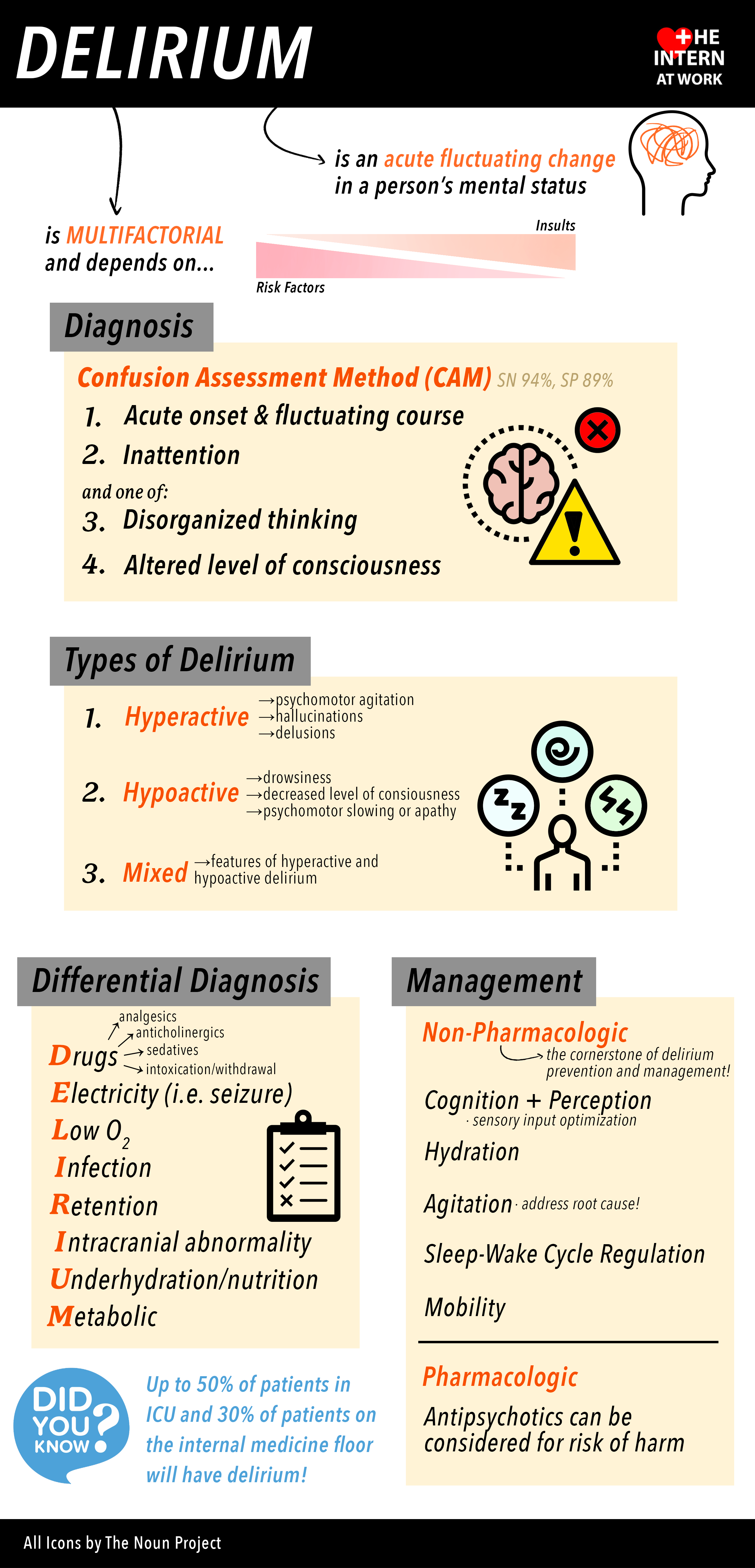
Diagnosed if patient has:
Inattention with acute onset and fluctuating course and disorganized thinking OR altered LOC.
Can present as hypo-, hyperactive or mixed delirium
Supportive features include sleep-wake cycle disturbance, hallucinations, delusions, increased or decreased psychomotor activity, inappropriate behavior, and emotional lability
Identification of etiology often requires collateral history as patients are unable to provide clear information themselves
Etiology - DIMERS mnemonic
Drugs
analgesics
anticholinergics
sedatives
nicotine withdrawal
alcohol intoxication or withdrawal
street drug intoxication or withdrawal
Infection
pneumonia
UTI - asymptomatic bacteriuria is hotly debated with respect to its role in pathogenesis of delirium; assess for any symptoms such as dysuria, frequency or suprapubic tenderness and use clinical judgement when deciding whether to treat if asymptomatic
cellulitis or skin ulcers
abscess
meningitis or encephalitis
Metabolic
electrolyte abnormalities - sodium, calcium, magnesium
hypo/hyperthyroidism
hepatic encephalopathy
renal encephalopathy
B12 deficiency
hypoxemia or hypercarbia
Environmental
unfamiliar environment
lack of visual or hearing aids
Retention
Constipation
Urinary Retention
Pain
Structural
stroke
ACS or CHF
Seizure
Treatment:
Focus on addressing identifiable causes and using non-pharmacologic interventions. Use of antipsychotics should be avoided as much as possible and limited to situations where patient or staff safety is a concern or patient is in significant distress.
re-orient frequently to time and place
where possible abort reversal of day/night cycles by having patient out of bed, facing sunlight during the day, lights off, earplugs and quiet room at night
minimize sensory deprivation by ensuring patient has their glasses, hearing aids, dentures, etc.
frequent visits from familiar family or friends if possible, use of elder life programs where available in hospital
encourage mobility, sitting up and out of bed for meals
avoid rapid discontinuation of chronic medications - for example, while benzodiazepines are a known risk fact0r for delirium and falls, abrupt discontinuation can also precipitate withdrawal and delirium
taper slowly, ideally in the outpatient setting using known guidelines
Medications: Should be reserved for instances where there is concern for patient or staff safety or severe distress. Chemical restraints favoured over physical restraints.
Quetiapine: 6.25-25mg po BID
agent of choice in patients with Parkinson’s or Lewy Body Dementia
Haloperidol: 0.25-1.0mg po BID (breakthrough q4h PRN), 0.25-1.0mg IM, can repeat q30-60min
can also be given IV but avoid where possible due to increased risk of arrhythmia and mortality
AVOID in patients with Parkinson’s or Lewy Body Dementia
Lorazepam: 0.5-1.0mg po
do NOT use routinely for delirium
indicated only in patients with alcohol or benzodiazepine withdrawal