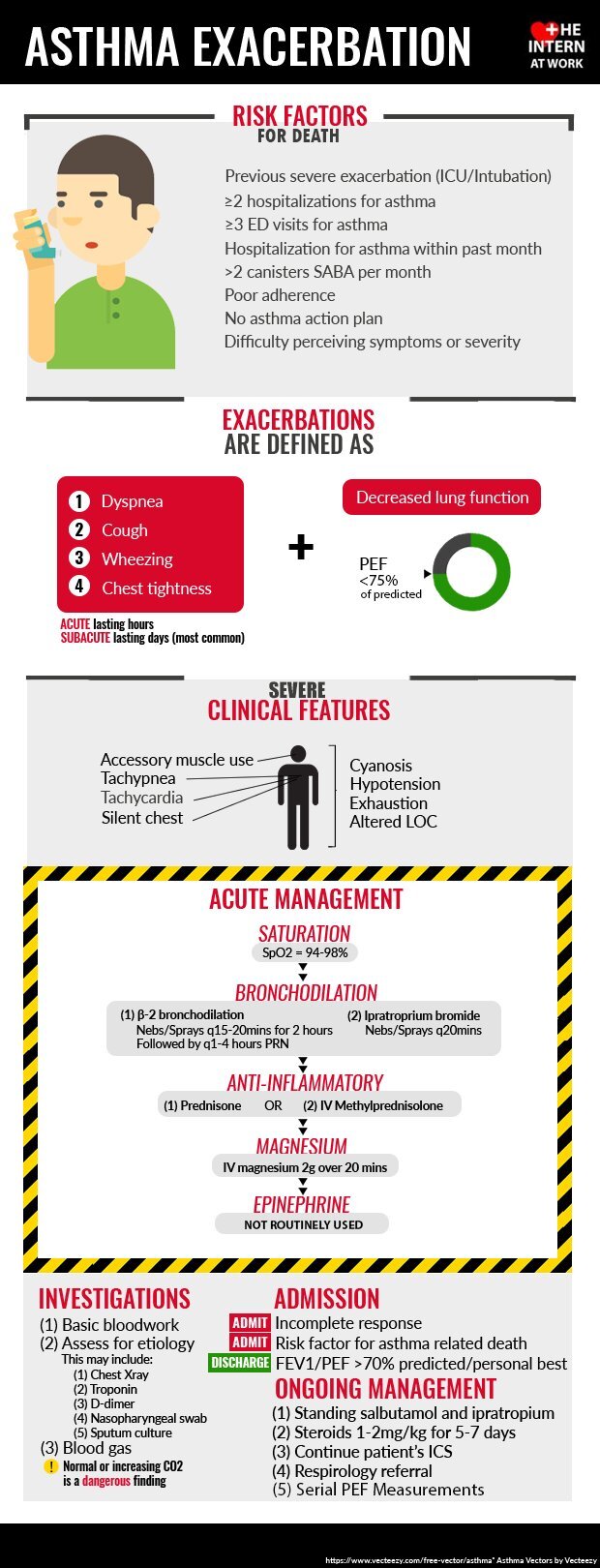
Day 2- Asthma Exacerbation
Assess for Stability
ABC’s
If severe or near death symptoms, CALL FOR HELP including critical care team and an advanced intubator!
Decision to intubate is clinical. Patients can decompensated quickly. Hypoxia is not commonly present in asthma exacerbations.
Severe: laboured breathing, agitated, diaphoretic, difficulty speaking, tachycardia, no relief with Beta agonists
Near death: exhausted, confused, dec LOC, cyanotic, silent chest, dec resp effort, dec HR
Oxygenation
O2 via NP or venturi to keep SaO2>94 %
Inhalers (Be generous)
Salbutamol (with nebulizer if available or ) q15min 1-2hrs then every 1-4 hrs PRN
Salbutamol (MDI with aero chamber) 100mcg 8puffs (repeat 15-20 min for 4 hrs then every 1-4hrs PRN)
If patient not responding, consider continuous nebulization at 5-10mg/hr if institution allows
+
Atrovent 0.5mg via nebulizer q20min then PRN
Atrovent 20mcg 8 puffs every 20 min for 3 hrs then PRN)
Steroids (Give ASAP, benefit can be seen in first hour)
Prednisone 40-50mg PO or IV methylprednisolone 125mg IV
Other
Avoid sedatives and narcotics
IV magnesium 2g in 250ml NS IV over 20 min (additional bronchodilator effect)
Routine use of Epinephrine not recommended in current guidelines
Use of NIV is contreversial (EBM link)
After exacerbation:
investigate triggers
PEF daily
salbutamol and ipatropium q4hrs while awake with salbutamol q1-2hr break-through dosing
Continue prednisone 1mg/kg for 5-7 days (some patients may require longer duration)
Continue inhaled corticosteroids in addition to oral (if patient is not on inhaled corticosteroids prescribe before discharge)
Arrange in-patient or out-patient Respirology follow-up
Can be discharged when PEF>70% or if symptoms minimal or absent