Day 1 - Transfusion Medicine
Informed Consent:
Informed consent must be documented physically in the patients chart and often also on hospital designated forms
Discuss: when treatment will occur, description of blood product, benefits (this may help with your symptoms of fatigue), risks (fever, anaphylaxis, bacterial infection, fluid overload, rare blood borne diseases), alternatives (no treatment, iron transfusion)
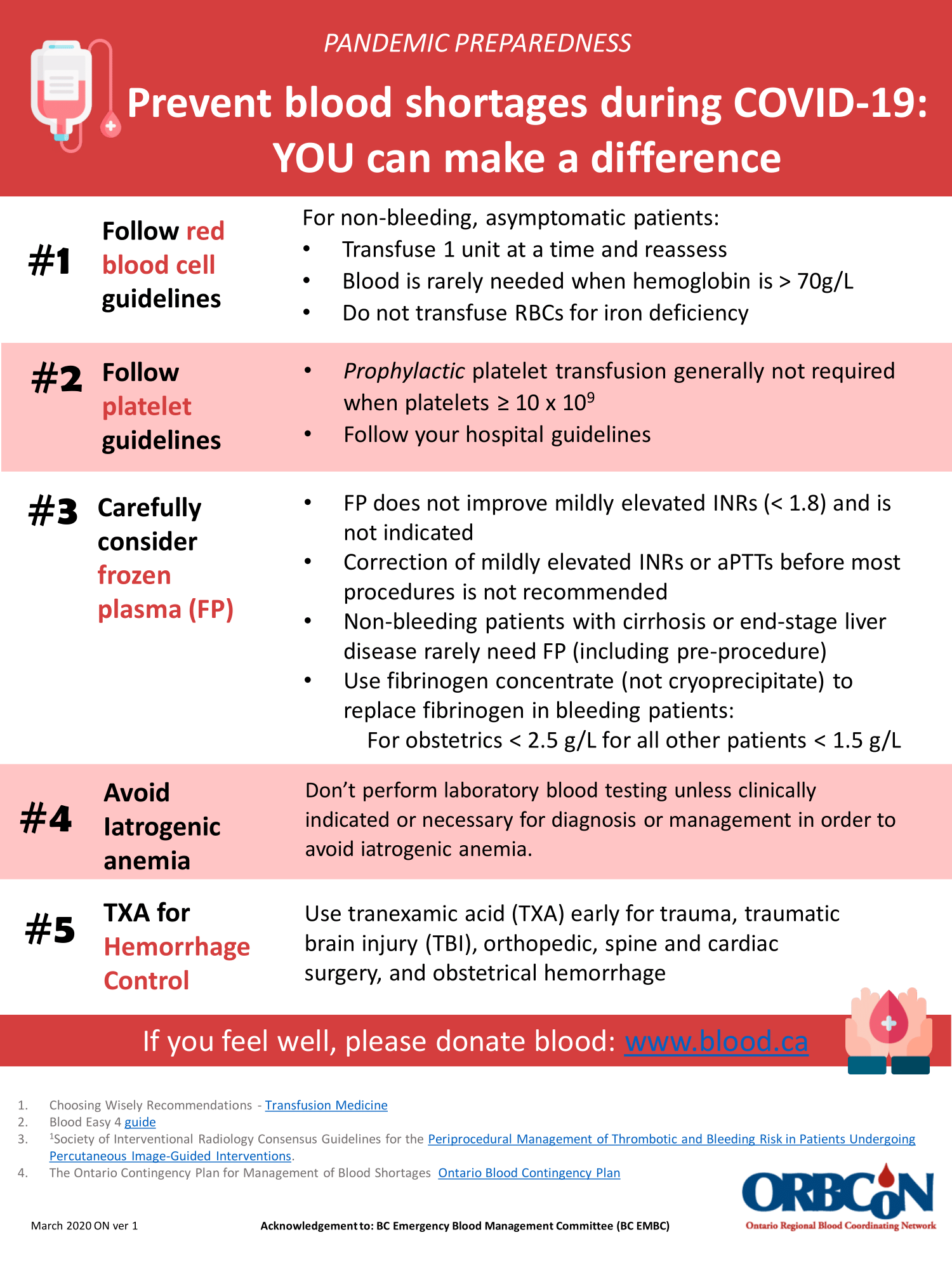
RBC Transfusion:
Consider transfusion when:
Hb<70g/L and active bleeding
Hb<80g/L (With coronary artery disease) and active bleeding
*(Consider use of tranxemic acid as well! Question whether this requires activation of a massive transfusion protocol)
Do not transfuse RBC’s to an asymptomatic, non-bleeding, inpatient with a hemoglobin level above 70g/L
Special considerations for procedures and surgeries not discussed here
*If Hb low, repeat CBC (margin of error 10g/L) and group and screen
*Typical dose: 1 unit of pRBC IV over 2 hours (consider lasix pre or post transfusion if concerned about overload)
Each unit of pRBC is expected to raise the Hb by approximately 10g/L
Platelet Transfusion:
Consider transfusion when:
Platelets <10 x 10^9
Platelets <20 x 10^9 and about to preform procedures not associated with significant blood loss (ie. central line)
Platelets <50 x 10^9 and about to preform procedures associated with significant blood loss (>500mL expected blood loss)
Platlets <100 x 10^9 pre-neurosurgery or head trauma
*Typical dose: 1 unit of platelets IV over 1 hour
*Monitor patient closely for the first 15 minutes especially for signs of bacterial sepsis
*Each dose of platelets should increase platelet count at 1 hour by at least 15-25 x 10^9/L